Oral Allergy Syndrome: Two Case Reports in Dental Practices
Abstract
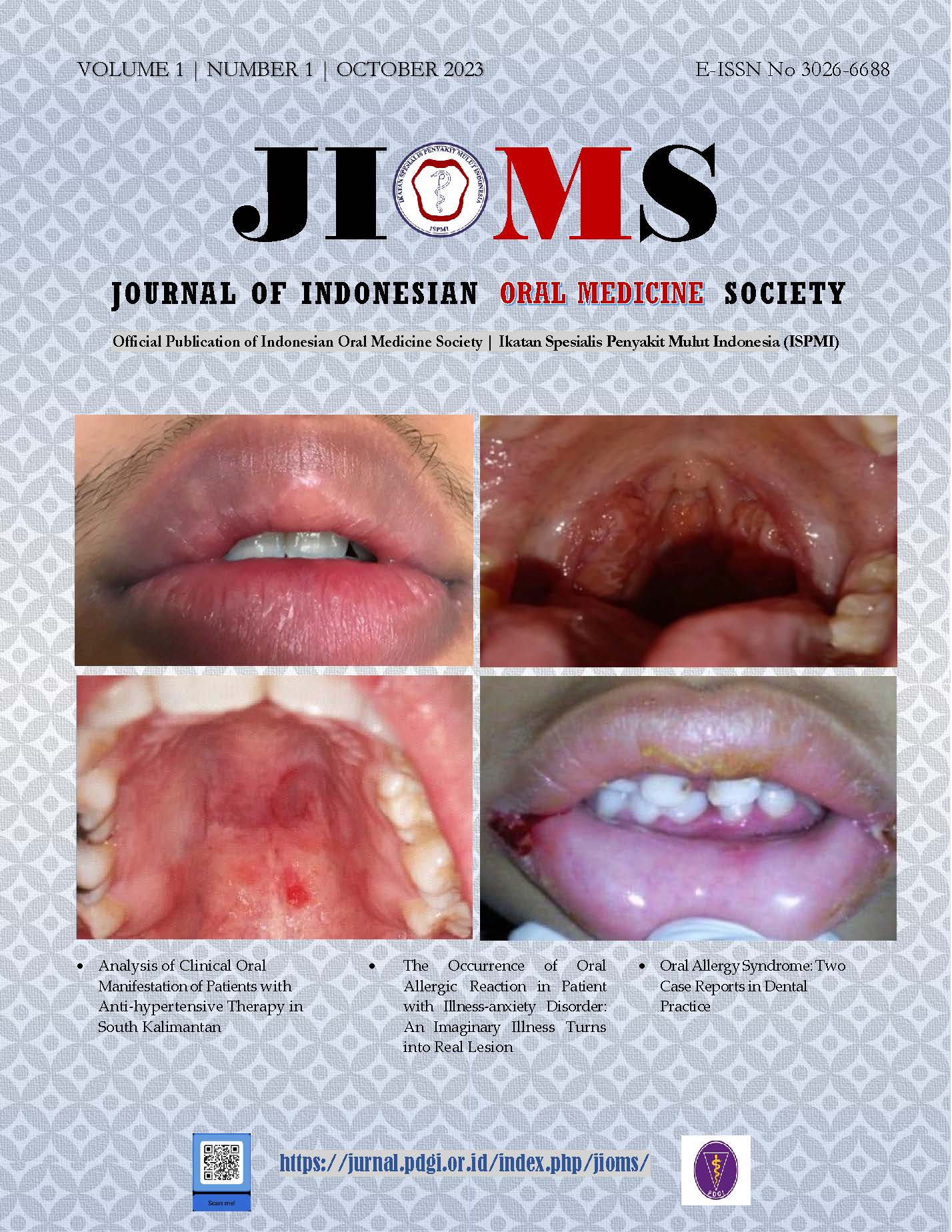
Background: Oral Allergy Syndrome (OAS) is a food allergic reaction towards fruit, vegetable and nut causing clinical symptoms in the form of itching, pain, vascular edema, and a narrow throat. In this case report, we reported management two cases of oral allergy syndrome due to banana and longan. Cases: The first case reported a 20-year-old man complaining of both upper and lower swollen lips after eating longan fruit. The second case was a 54-year-old woman complaining of pain and discomfort in the upper lip, mouth corners, left and right inner cheeks, palate and especially on the tongue. She had had an Ambon Banana the day before. Case Management: Both patients were given antihistamine treatment and informed to avoid the suspected fruits which caused the allergic reaction. The diagnosis is established using the oral food challenge method. Conclusion: The principle of management of OAS cases is to identify and avoid allergens. Antihistamines are the drug of choice for this case.References
1. American Academy of Allergy Asthma & Imunology. Oral Allergy Syndrome – Pollens and Cross-Reacting Foods Table.; 2019.
2. Muluk NB, Cingi C. Oral allergy syndrome. Am J Rhinol Allergy. 2018;32(1):27-30. doi:10.2500/ajra.2018.32.4489
3. Zhang Md Y, Marzouk Md H. Otolaryngologists Practice Pattern on Oral Allergy Syndrome. Allergy Rhinol (Providence). 2021;12:21526567211021304. doi:10.1177/21526567211021305
4. Högerle C, Nicolo MS, Gellrich D, Eder K, Gröger M. Clinical Relevance of Profilin Sensitization Concerning Oral Allergy Syndrome in Birch Pollen Sensitized Patients. J Asthma Allergy. 2022;15(January):249-255. doi:10.2147/JAA.S348650
5. Skypala IJ, Hunter H, Krishna MT, et al. BSACI guideline for the diagnosis and management of pollen food syndrome in the UK. Clin Exp Allergy. 2022;52(9):1018-1034. doi:https://doi.org/10.1111/cea.14208
6. Carlson G, Coop C. Pollen food allergy syndrome (PFAS): A review of current available literature. Ann allergy, asthma Immunol Off Publ Am Coll Allergy, Asthma, Immunol. 2019;123(4):359-365. doi:10.1016/j.anai.2019.07.022
7. Mastrorilli C, Cardinale F, Giannetti A, Caffarelli C. Pollen-Food Allergy Syndrome: A not so Rare Disease in Childhood. Medicina (Kaunas). 2019;55(10). doi:10.3390/medicina55100641
8. Skypala IJ. Can patients with oral allergy syndrome be at risk of anaphylaxis? Curr Opin Allergy Clin Immunol. 2020;20(5):459-464. doi:10.1097/ACI.0000000000000679
9. Pier J, Bingemann TA. Urticaria, Angioedema, and Anaphylaxis. Pediatr Rev. 2020;41(6):283-292. doi:10.1542/pir.2019-0056
10. Calvani M, Bianchi A, Reginelli C, Peresso M, Testa A. Oral Food Challenge. Medicina (Kaunas). 2019;55(10). doi:10.3390/medicina55100651
11. Alessandri C, Alessandri C, Ferrara R, et al. Molecular approach to a patient’s tailored diagnosis of the oral allergy syndrome. Clin Transl Allergy. 2020;10(1):1-18. doi:10.1186/s13601-020-00329-8
12. Sharma L, Agarwal R, Chopra A, Mitra B. A Cross-Sectional Observational Study of Clinical Spectrum and Prevalence of Fixed Food Eruption in a Tertiary Care Hospital. Indian Dermatol Online J. 2020;11(3):361-366. doi:10.4103/idoj.IDOJ_340_19
13. Sohn KH, Kim BK, Kim JY, et al. Fixed Food Eruption Caused by Actinidia arguta (Hardy Kiwi): A Case Report and Literature Review. Allergy Asthma Immunol Res. 2017;9(2):182-184. doi:10.4168/aair.2017.9.2.182
14. Shaker MS, Wallace D V, Golden DBK, et al. Anaphylaxis-a 2020 practice parameter update, systematic review, and Grading of Recommendations, Assessment, Development and Evaluation (GRADE) analysis. J Allergy Clin Immunol. 2020;145(4):1082-1123. doi:10.1016/j.jaci.2020.01.017
15. Pflipsen MC, Vega Colon KM. Anaphylaxis: Recognition and Management. Am Fam Physician. 2020;102(6):355-362.
16. Naqvi A, Gerriets V. Cetirizine. In: ; 2022.
17. Zhou P, Jia Q, Wang Z, Zhao R, Zhou W. Cetirizine for the treatment of allergic diseases in children: A systematic review and meta-analysis. Front Pediatr. 2022;10:940213. doi:10.3389/fped.2022.940213
18. Adusumilli NC, Friedman AJ. An Updated Therapeutic Strategy for Chronic Idiopathic Urticaria. J Drugs Dermatol. 2021;20(3):354-355. doi:10.36849/JDD.0421
19. Bird JA, Leonard S, Groetch M, et al. Conducting an Oral Food Challenge: An Update to the 2009 Adverse Reactions to Foods Committee Work Group Report. J allergy Clin Immunol Pract. 2020;8(1):75-90.e17. doi:10.1016/j.jaip.2019.09.029
20. Nachshon L, Zipper O, Levy MB, Goldberg MR, Epstein-Rigby N, Elizur A. Subjective oral symptoms are insufficient predictors of a positive oral food challenge. Pediatr allergy Immunol Off Publ Eur Soc Pediatr Allergy Immunol. 2021;32(2):342-348. doi:10.1111/pai.13392
2. Muluk NB, Cingi C. Oral allergy syndrome. Am J Rhinol Allergy. 2018;32(1):27-30. doi:10.2500/ajra.2018.32.4489
3. Zhang Md Y, Marzouk Md H. Otolaryngologists Practice Pattern on Oral Allergy Syndrome. Allergy Rhinol (Providence). 2021;12:21526567211021304. doi:10.1177/21526567211021305
4. Högerle C, Nicolo MS, Gellrich D, Eder K, Gröger M. Clinical Relevance of Profilin Sensitization Concerning Oral Allergy Syndrome in Birch Pollen Sensitized Patients. J Asthma Allergy. 2022;15(January):249-255. doi:10.2147/JAA.S348650
5. Skypala IJ, Hunter H, Krishna MT, et al. BSACI guideline for the diagnosis and management of pollen food syndrome in the UK. Clin Exp Allergy. 2022;52(9):1018-1034. doi:https://doi.org/10.1111/cea.14208
6. Carlson G, Coop C. Pollen food allergy syndrome (PFAS): A review of current available literature. Ann allergy, asthma Immunol Off Publ Am Coll Allergy, Asthma, Immunol. 2019;123(4):359-365. doi:10.1016/j.anai.2019.07.022
7. Mastrorilli C, Cardinale F, Giannetti A, Caffarelli C. Pollen-Food Allergy Syndrome: A not so Rare Disease in Childhood. Medicina (Kaunas). 2019;55(10). doi:10.3390/medicina55100641
8. Skypala IJ. Can patients with oral allergy syndrome be at risk of anaphylaxis? Curr Opin Allergy Clin Immunol. 2020;20(5):459-464. doi:10.1097/ACI.0000000000000679
9. Pier J, Bingemann TA. Urticaria, Angioedema, and Anaphylaxis. Pediatr Rev. 2020;41(6):283-292. doi:10.1542/pir.2019-0056
10. Calvani M, Bianchi A, Reginelli C, Peresso M, Testa A. Oral Food Challenge. Medicina (Kaunas). 2019;55(10). doi:10.3390/medicina55100651
11. Alessandri C, Alessandri C, Ferrara R, et al. Molecular approach to a patient’s tailored diagnosis of the oral allergy syndrome. Clin Transl Allergy. 2020;10(1):1-18. doi:10.1186/s13601-020-00329-8
12. Sharma L, Agarwal R, Chopra A, Mitra B. A Cross-Sectional Observational Study of Clinical Spectrum and Prevalence of Fixed Food Eruption in a Tertiary Care Hospital. Indian Dermatol Online J. 2020;11(3):361-366. doi:10.4103/idoj.IDOJ_340_19
13. Sohn KH, Kim BK, Kim JY, et al. Fixed Food Eruption Caused by Actinidia arguta (Hardy Kiwi): A Case Report and Literature Review. Allergy Asthma Immunol Res. 2017;9(2):182-184. doi:10.4168/aair.2017.9.2.182
14. Shaker MS, Wallace D V, Golden DBK, et al. Anaphylaxis-a 2020 practice parameter update, systematic review, and Grading of Recommendations, Assessment, Development and Evaluation (GRADE) analysis. J Allergy Clin Immunol. 2020;145(4):1082-1123. doi:10.1016/j.jaci.2020.01.017
15. Pflipsen MC, Vega Colon KM. Anaphylaxis: Recognition and Management. Am Fam Physician. 2020;102(6):355-362.
16. Naqvi A, Gerriets V. Cetirizine. In: ; 2022.
17. Zhou P, Jia Q, Wang Z, Zhao R, Zhou W. Cetirizine for the treatment of allergic diseases in children: A systematic review and meta-analysis. Front Pediatr. 2022;10:940213. doi:10.3389/fped.2022.940213
18. Adusumilli NC, Friedman AJ. An Updated Therapeutic Strategy for Chronic Idiopathic Urticaria. J Drugs Dermatol. 2021;20(3):354-355. doi:10.36849/JDD.0421
19. Bird JA, Leonard S, Groetch M, et al. Conducting an Oral Food Challenge: An Update to the 2009 Adverse Reactions to Foods Committee Work Group Report. J allergy Clin Immunol Pract. 2020;8(1):75-90.e17. doi:10.1016/j.jaip.2019.09.029
20. Nachshon L, Zipper O, Levy MB, Goldberg MR, Epstein-Rigby N, Elizur A. Subjective oral symptoms are insufficient predictors of a positive oral food challenge. Pediatr allergy Immunol Off Publ Eur Soc Pediatr Allergy Immunol. 2021;32(2):342-348. doi:10.1111/pai.13392
Published
2023-11-01
How to Cite
MUJAYANTO, Rochman; ALMAS, Mazaya; WISAPUTRI, Devina Vedayumna.
Oral Allergy Syndrome: Two Case Reports in Dental Practices.
Journal of Indonesian Oral Medicine Society, [S.l.], v. 1, n. 1, p. 14-18, nov. 2023.
ISSN 3026-6688.
Available at: <http://jurnal.pdgi.or.id/index.php/jioms/article/view/1098>. Date accessed: 10 mar. 2026.
Section
Case Reports