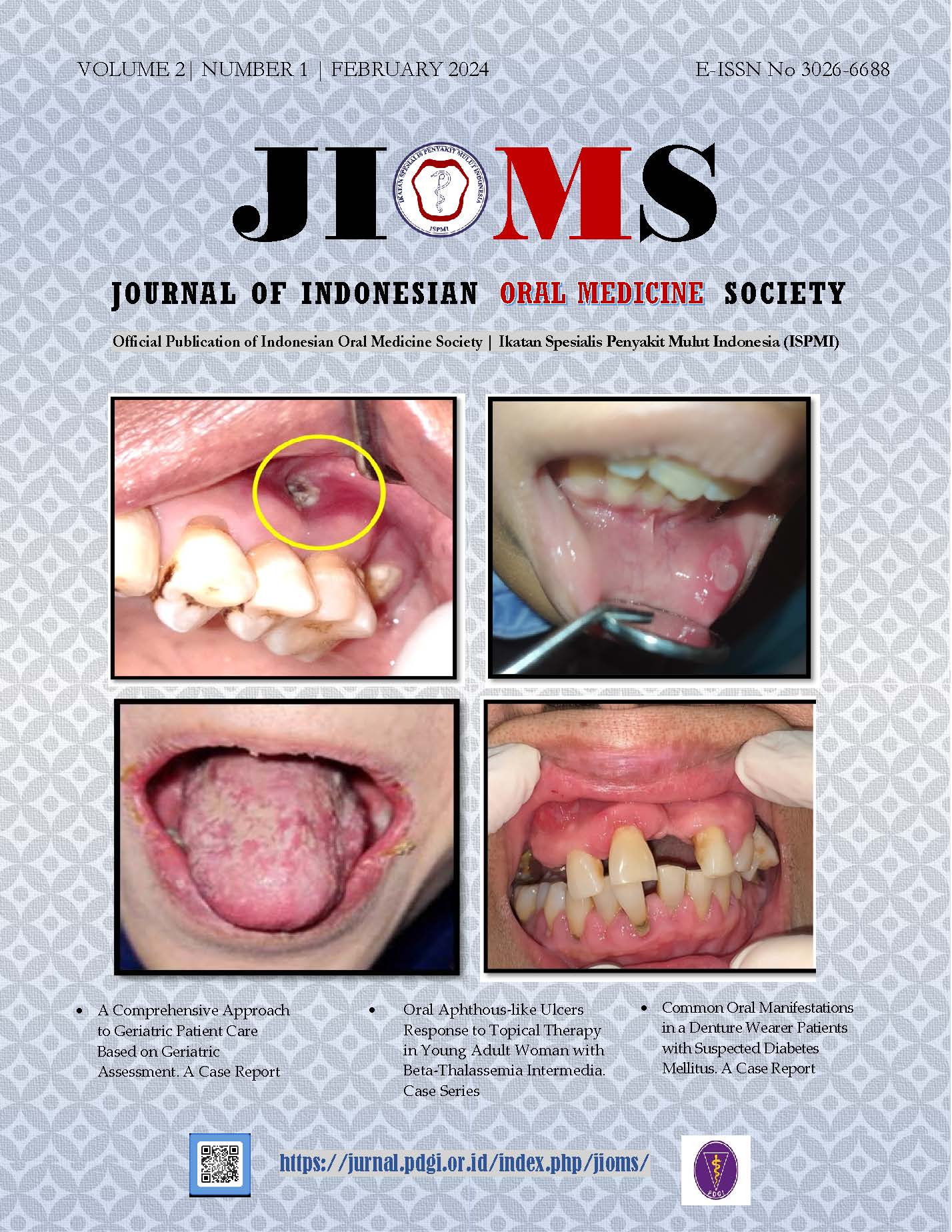
Oral Aphthous-like Ulcers Response to Topical Therapy in Young Adult Woman with Beta-Thalassemia Intermedia
Abstract
Background: Beta thalassemia may have some oral manifestations. Oral mucosa ulcer may be one of the oral manifestations of beta-thalassemia. The oral ulcer may resemble recurrent aphthous stomatitis (RAS). This current case report aims to present an aphthous oral ulcer as a manifestation in young adult women with beta-thalassemia. Case report: A 28-year-old woman complained of recurrent painful oral ulcers in the labial mucosa. She was diagnosed with beta-thalassemia intermedia three years before. The ulcer may take 3-4 weeks to heal completely. Intraoral examination revealed two yellowish ulcers, 5 mm and 10 mm, surrounded by an erythematous halo, regular margin on left lips mucosa, oral ulcer pain scale measured medium level by visual analogue scale (VAS). The oral aphthous-like ulcer was taken for diagnosis in this case. Topical treatment was given to the oral ulcer using chlorine dioxide gel three times daily. After 10 days, the oral aphthous-like ulcer was healed. Conclusion: An oral aphthous-like ulcer may be the oral manifestation in beta-thalassemia patients, and the oral ulcer may respond well to topical treatment commonly used in recurrent aphthous stomatitis (RAS) patients. Hence, it is important to recognize oral conditions as one clinical manifestation in beta-thalassemia patients and choose the appropriate treatment to accelerate oral ulcer healing.References
1. Origa, R. (2017). β-Thalassemia. In Genetics in Medicine (Vol. 19, Issue 6, pp. 609–619). Nature Publishing Group. https://doi.org/10.1038/gim.2016.173
2. Hattab, F. N. (2013). Pattern of Physical growth and dental development in Jordanian children and adolescents with thalassemia major. Journal of Oral Science, 55(1), 71–77.
3. Raeesi, A., Kowash, S. B., & Halabi, A. (2017). Medical and Dental Implications of Patients with Beta Thalassaemia Major. Part 2: Orofacial and Dental Characteristics: A Review. JSM Dent, 5(2), 1092-1–96.
4. Riyanti, E. (2008). Dental and oral management in beta major thalassemia in children. Padjajaran Journal of Dentistry, 20(1), 43–48.
5. Arora, A., & Sathyaprasad, S. (2022). Oro-facial Manifestations, Oral Health Status and Treatment Needs in Transfusion Dependent Children With β-thalassemia Major: A Cross-sectional Study. Malaysian Journal of Medicine and Health Sciences, 18(2), 76–80.
6. Abulsattar, M. S., & Al-Yassiri, A. M. (2014). Prevalence of Orofacial changes in patients with Beta-thalassemia major in Karbala City, Iraq. Seluaimani Dental Journal, 1, 64–67.
7. Rahim Abdulkarim, D., & M. Gaphor, S. (2023). Prevalence of Oral Manifestation of Thalassemic Patients in Sulaymaniyah Thalassemia Center. Tikrit Journal for Dental Sciences, 11(1), 93–104. https://doi.org/10.25130/tjds.11.1.11
8. Amirabadi, F., Saravani, S., Miri-Aliabad, G., & Khorashadi-Zadeh, M. (2019). The Association between Dental Health Status and Oral Health-Related Quality of Life of Children Diagnosed with -Thalassemia Major in Zahedan City, Iran. Int J Pediatr, 7(2), 8985–8991. https://doi.org/10.22038/ijp.2018.34517.3034
9. Nabi, A., Muttu, J., Chhaparwal, A., Mukhopadhyay, A., Pattnaik, S., & Choudhary, P. (2022). Implications of β-thalassemia on oral health status in patients: A cross-sectional study. Journal of Family Medicine and Primary Care, 11(3), 1174–1178. https://doi.org/10.4103/jfmpc.jfmpc_1215_21
10. Nagaveni, N. B., P, P., & Koley, P. (2017). Clinical Management of a Pediatric Patient Associated with Thalassemia Major: A Case Report. CODS Journal of Dentistry, 9(2), 55–58. https://doi.org/10.5005/jp-journals-10063-0034
11. Widodo, H. B., & Maharani, A. E. (2019). Oral manifestation of thalassemia Beta mayor: case study. Journal of Case Reports in Dental Medicine, 1(2), 32–35. https://doi.org/10.20956/jcrdm.v1i2.90
12. Vesna, A., Tina, K., & Zoran, N. (2021). Thalassemia-Beta Major-Case report. Archives of Hematology Case Reports and Reviews, 021–025. https://doi.org/10.17352/ahcrr.000034
13. Riyanto, D., Soebadi, B., Hadi, P., & Radithia, D. (2020). Management of aphthous-like ulcer induce by trauma in a patient with thalassemia beta intermedia: a case report. Journal of Case Reports in Dental Medicine, 2(1), 5–8. https://doi.org/10.20956/jcrdm.v2i1.110
14. Namrata, M., & Abilasha, R. (2017). Recurrent Aphthous Stomatitis. International Journal of Orofacial Biology, 1(1), 43–47. https://doi.org/10.4103/ijofb.ijofb
15. Oyetola, E. O., Mogaji, I. K., Aghor, T. O., & O.A Ayilara. (2018). Pattern of Presentation of Oral Ulceration in Patients Attending an Oral Medicine Clinic in Nigeria. Annals of Ibadan Postgraduate Medicine, 16(1), 9–11.
16. Verma, S., Srikrishna, K., S., Shalini, K., Sinha, G., & Srivastava, P. (2023). Recurrent Oral Ulcers and Its Association with Stress Among Dental Students in the Northeast Indian Population: A Cross-Sectional Questionnaire-Based Survey. Cureus, 15(2), 1–10. https://doi.org/10.7759/cureus.34947
17. Seizer, L., & Schubert, C. (2022). On the Role of Psychoneuroimmunology in Oral Medicine. In International Dental Journal (Vol. 72, Issue 6, pp. 765–772). Elsevier Inc. https://doi.org/10.1016/j.identj.2022.07.002
18. Challacombe, S. J., Alsahaf, S., & Tappuni, A. (2015). Recurrent Aphthous Stomatitis: Towards Evidence-Based Treatment? Current Oral Health Reports, 2, 158–167. https://doi.org/10.1007/s40496-015-0054-y
19. Wu, Y. C., Wu, Y. H., Wang, Y. P., Chang, J. Y. F., Chen, H. M., & Sun, A. (2016). Hematinic deficiencies and anemia statuses in recurrent aphthous stomatitis patients with or without atrophic glossitis. Journal of the Formosan Medical Association, 115(12), 1061–1068. https://doi.org/10.1016/j.jfma.2016.10.007
20. Akintoye, S. O., & Greenberg, M. S. (2014). Recurrent Aphthous Stomatitis. Dental Clinics of North America, 58(2), 281–297. https://doi.org/10.1016/j.cden.2013.12.002.Recurrent
21. Kerémi, B., Márta, K., Farkas, K., Czumbel, L. M., Tóth, B., Szakács, Z., Csupor, D., Czimmer, J., Rumbus, Z., Révész, P., Németh, A., Gerber, G., Hegyi, P., & Varga, G. (2020). Effects of Chlorine Dioxide on Oral Hygiene - A Systematic Review and Meta-analysis. Current Pharmaceutical Design, 26(25), 3015–3025. https://doi.org/10.2174/1381612826666200515134450
22. Mani, S. (2012). Chlorine Dioxide: A Potential Mouth Rinse for Oral Health. International Journal of Experimental Dental Science, 1(2), 118–119. https://doi.org/10.5005/jp-journals-10029-1029
23. Peredo-Lovillo, A., Romero-Luna, H. E., Juárez-Trujillo, N., & Jiménez-Fernández, M. (2023). Antimicrobial efficiency of chlorine dioxide and its potential use as anti-SARS-CoV-2 agent: mechanisms of action and interactions with gut microbiota. Journal of Applied Microbiology, 134(7), 1–13. https://doi.org/10.1093/jambio/lxad133
24. Lin, P. H., Sermersheim, M., Li, H., Lee, P. H. U., Steinberg, S. M., & Ma, J. (2018). Zinc in wound healing modulation. Nutrients, 10(16), 2–20. https://doi.org/10.3390/nu10010016
25. Permatasanti, A., Fitriasari, N., Sari, N. M., & Wahyuni, I. S. (2023). Antioxidant Effect of Mouthwash Containing Zinz, Aloe Vera, and Stabilized Chlorine Dioxide for Oral Manifestation of Acute Myeloblastic Leukemia (AML). International Journal of Applied Pharmaceutics, 15(Special Issue 2), 58–62. https://doi.org/10.22159/ijap.2023.v15s2.11
2. Hattab, F. N. (2013). Pattern of Physical growth and dental development in Jordanian children and adolescents with thalassemia major. Journal of Oral Science, 55(1), 71–77.
3. Raeesi, A., Kowash, S. B., & Halabi, A. (2017). Medical and Dental Implications of Patients with Beta Thalassaemia Major. Part 2: Orofacial and Dental Characteristics: A Review. JSM Dent, 5(2), 1092-1–96.
4. Riyanti, E. (2008). Dental and oral management in beta major thalassemia in children. Padjajaran Journal of Dentistry, 20(1), 43–48.
5. Arora, A., & Sathyaprasad, S. (2022). Oro-facial Manifestations, Oral Health Status and Treatment Needs in Transfusion Dependent Children With β-thalassemia Major: A Cross-sectional Study. Malaysian Journal of Medicine and Health Sciences, 18(2), 76–80.
6. Abulsattar, M. S., & Al-Yassiri, A. M. (2014). Prevalence of Orofacial changes in patients with Beta-thalassemia major in Karbala City, Iraq. Seluaimani Dental Journal, 1, 64–67.
7. Rahim Abdulkarim, D., & M. Gaphor, S. (2023). Prevalence of Oral Manifestation of Thalassemic Patients in Sulaymaniyah Thalassemia Center. Tikrit Journal for Dental Sciences, 11(1), 93–104. https://doi.org/10.25130/tjds.11.1.11
8. Amirabadi, F., Saravani, S., Miri-Aliabad, G., & Khorashadi-Zadeh, M. (2019). The Association between Dental Health Status and Oral Health-Related Quality of Life of Children Diagnosed with -Thalassemia Major in Zahedan City, Iran. Int J Pediatr, 7(2), 8985–8991. https://doi.org/10.22038/ijp.2018.34517.3034
9. Nabi, A., Muttu, J., Chhaparwal, A., Mukhopadhyay, A., Pattnaik, S., & Choudhary, P. (2022). Implications of β-thalassemia on oral health status in patients: A cross-sectional study. Journal of Family Medicine and Primary Care, 11(3), 1174–1178. https://doi.org/10.4103/jfmpc.jfmpc_1215_21
10. Nagaveni, N. B., P, P., & Koley, P. (2017). Clinical Management of a Pediatric Patient Associated with Thalassemia Major: A Case Report. CODS Journal of Dentistry, 9(2), 55–58. https://doi.org/10.5005/jp-journals-10063-0034
11. Widodo, H. B., & Maharani, A. E. (2019). Oral manifestation of thalassemia Beta mayor: case study. Journal of Case Reports in Dental Medicine, 1(2), 32–35. https://doi.org/10.20956/jcrdm.v1i2.90
12. Vesna, A., Tina, K., & Zoran, N. (2021). Thalassemia-Beta Major-Case report. Archives of Hematology Case Reports and Reviews, 021–025. https://doi.org/10.17352/ahcrr.000034
13. Riyanto, D., Soebadi, B., Hadi, P., & Radithia, D. (2020). Management of aphthous-like ulcer induce by trauma in a patient with thalassemia beta intermedia: a case report. Journal of Case Reports in Dental Medicine, 2(1), 5–8. https://doi.org/10.20956/jcrdm.v2i1.110
14. Namrata, M., & Abilasha, R. (2017). Recurrent Aphthous Stomatitis. International Journal of Orofacial Biology, 1(1), 43–47. https://doi.org/10.4103/ijofb.ijofb
15. Oyetola, E. O., Mogaji, I. K., Aghor, T. O., & O.A Ayilara. (2018). Pattern of Presentation of Oral Ulceration in Patients Attending an Oral Medicine Clinic in Nigeria. Annals of Ibadan Postgraduate Medicine, 16(1), 9–11.
16. Verma, S., Srikrishna, K., S., Shalini, K., Sinha, G., & Srivastava, P. (2023). Recurrent Oral Ulcers and Its Association with Stress Among Dental Students in the Northeast Indian Population: A Cross-Sectional Questionnaire-Based Survey. Cureus, 15(2), 1–10. https://doi.org/10.7759/cureus.34947
17. Seizer, L., & Schubert, C. (2022). On the Role of Psychoneuroimmunology in Oral Medicine. In International Dental Journal (Vol. 72, Issue 6, pp. 765–772). Elsevier Inc. https://doi.org/10.1016/j.identj.2022.07.002
18. Challacombe, S. J., Alsahaf, S., & Tappuni, A. (2015). Recurrent Aphthous Stomatitis: Towards Evidence-Based Treatment? Current Oral Health Reports, 2, 158–167. https://doi.org/10.1007/s40496-015-0054-y
19. Wu, Y. C., Wu, Y. H., Wang, Y. P., Chang, J. Y. F., Chen, H. M., & Sun, A. (2016). Hematinic deficiencies and anemia statuses in recurrent aphthous stomatitis patients with or without atrophic glossitis. Journal of the Formosan Medical Association, 115(12), 1061–1068. https://doi.org/10.1016/j.jfma.2016.10.007
20. Akintoye, S. O., & Greenberg, M. S. (2014). Recurrent Aphthous Stomatitis. Dental Clinics of North America, 58(2), 281–297. https://doi.org/10.1016/j.cden.2013.12.002.Recurrent
21. Kerémi, B., Márta, K., Farkas, K., Czumbel, L. M., Tóth, B., Szakács, Z., Csupor, D., Czimmer, J., Rumbus, Z., Révész, P., Németh, A., Gerber, G., Hegyi, P., & Varga, G. (2020). Effects of Chlorine Dioxide on Oral Hygiene - A Systematic Review and Meta-analysis. Current Pharmaceutical Design, 26(25), 3015–3025. https://doi.org/10.2174/1381612826666200515134450
22. Mani, S. (2012). Chlorine Dioxide: A Potential Mouth Rinse for Oral Health. International Journal of Experimental Dental Science, 1(2), 118–119. https://doi.org/10.5005/jp-journals-10029-1029
23. Peredo-Lovillo, A., Romero-Luna, H. E., Juárez-Trujillo, N., & Jiménez-Fernández, M. (2023). Antimicrobial efficiency of chlorine dioxide and its potential use as anti-SARS-CoV-2 agent: mechanisms of action and interactions with gut microbiota. Journal of Applied Microbiology, 134(7), 1–13. https://doi.org/10.1093/jambio/lxad133
24. Lin, P. H., Sermersheim, M., Li, H., Lee, P. H. U., Steinberg, S. M., & Ma, J. (2018). Zinc in wound healing modulation. Nutrients, 10(16), 2–20. https://doi.org/10.3390/nu10010016
25. Permatasanti, A., Fitriasari, N., Sari, N. M., & Wahyuni, I. S. (2023). Antioxidant Effect of Mouthwash Containing Zinz, Aloe Vera, and Stabilized Chlorine Dioxide for Oral Manifestation of Acute Myeloblastic Leukemia (AML). International Journal of Applied Pharmaceutics, 15(Special Issue 2), 58–62. https://doi.org/10.22159/ijap.2023.v15s2.11
Published
2024-02-29
How to Cite
SUSANTO, Hendri; DEWI, Rona Tirtaardi; HARDIANTI, Mardiah Suci.
Oral Aphthous-like Ulcers Response to Topical Therapy in Young Adult Woman with Beta-Thalassemia Intermedia.
Journal of Indonesian Oral Medicine Society, [S.l.], v. 2, n. 1, p. 8-13, feb. 2024.
ISSN 3026-6688.
Available at: <http://jurnal.pdgi.or.id/index.php/jioms/article/view/1157>. Date accessed: 14 feb. 2026.
doi: https://doi.org/10.32793/jioms.v2i1.1157.
Section
Case Reports

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.